
SGLT-2 inhibitors and sulfonylurea compounds may, under certain conditions, increase glucagon levels, however, within the physiological range ( 21, 33). The effects of glucose-lowering therapies on glucagon secretion are in general poorly understood-in particular, long-term effects and effects of older therapies ( 33). The secretion from extrapancreatic sources of glucagon remains to be fully described ( 2). Plasma glucose is an important and well-characterized regulator ( 19, 31), but recent evidence suggests that plasma amino acids may play an even more important role ( 32). Stimuli acting on the pancreatic alpha cell regulate glucagon secretion: neural, hormonal, and local paracrine factors, possibly including glucagon itself, amylin, insulin, somatostatin, and incretin hormones ( 27–30). Embase was searched for full-text articles using the string *glucagon/ or *glucagon blood level/ AND exp hemodynamic parameters/ or exp hemodynamic stress/ or hemodynamics/ AND Human/, and the Cochrane Library database was searched using the single key word “glucagon,” yielding no additional studies. Twenty-four human studies reporting hemodynamic effects of glucagon were identified and included ( Supplemental Tables 1 and 2). Reference searches were conducted in retrieved articles.
An article was included if it reported effects of a defined glucagon dose on a hemodynamic parameter measured at specified time points (no year restrictions). Methodsĭifferent search strategies were applied to identify studies on the hemodynamic effects of glucagon: in September 2017, we searched the PubMed database for full-text articles reporting human clinical studies investigating glucagon with the search string (((((((((glucagon) OR “Glucagon”) OR glucagon(title)) OR “Glucagon”))) NOT ((glucagon like peptide 1) OR Glucagon-Like Peptide 1 ))) AND ((((((“Cardiac Output/drug effects”) OR “Blood Pressure/drug effects”) OR “Hemodynamics/drug effects”) OR “Heart Ventricles/drug effects”) OR “Cardiovascular System/drug effects”) OR “Heart Rate/drug effects”)) AND (((((((“Humans”) OR “Clinical Study”)) OR human) OR man) OR trial)). We therefore reviewed and evaluated the literature regarding the pharmacology of glucagon with a focus on clinical hemodynamic effects. Altogether, understanding the consequences of increased glucagon levels on the cardiovascular system has become increasingly important. Cardiovascular effects of pharmacological treatments of obesity and type 2 diabetes are important the unexpected increase in cardiovascular risk with rosiglitazone was a clear example thereof ( 26). Increased glucagon levels may be harmful due to possible chronic tachycardia ( 23, 24), which in and of itself is a risk factor for cardiovascular morbidity ( 25). Thus, glucagon receptor activation may have a bearing on the hemodynamic effects and cardiovascular safety of these therapies. Furthermore, some current diabetes therapies, which have been found to improve cardiovascular outcomes in type 2 diabetes, increase endogenous glucagon secretion ( 20–22).

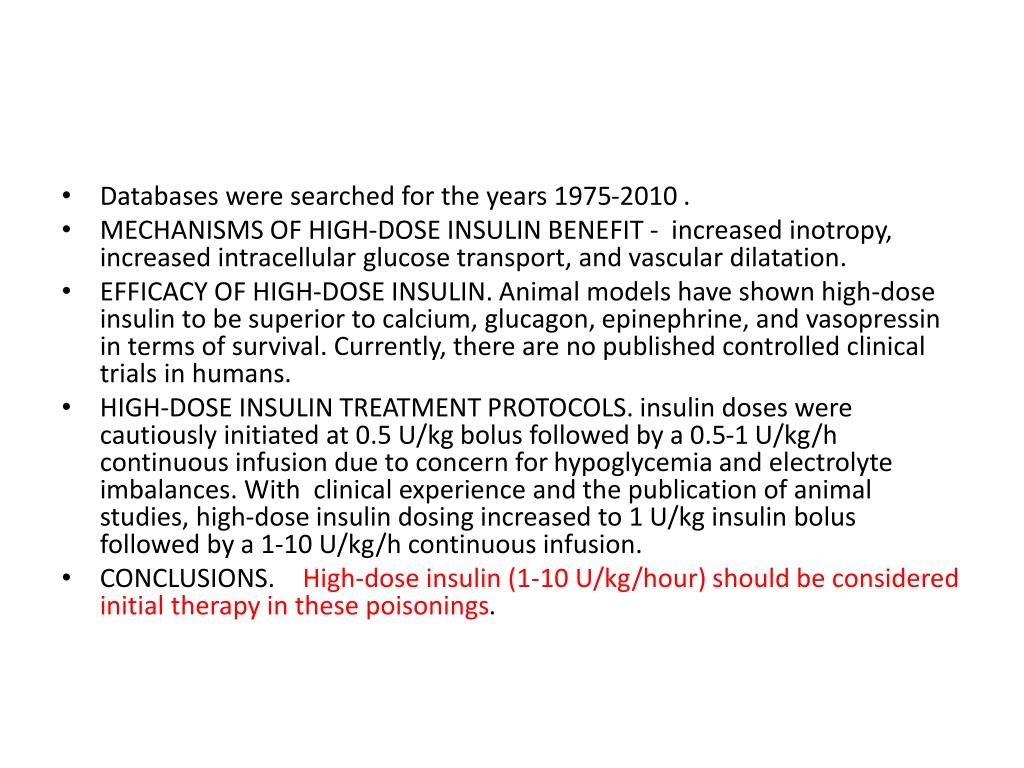
Recently, a renewed focus on glucagon signaling has emerged because the glucagon receptor is a key element in new and emerging treatments for obesity and type 2 diabetes ( 16): glucagon-like peptide 1 (GLP-1)/glucagon co-agonists are under investigation as potential therapy for obesity and type 2 diabetes ( 17, 18), and diabetes therapy based on closed-loop artificial pancreas systems is emerging ( 19). However, the actions of glucagon go beyond glucose homeostasis and involve direct effects on the cardiovascular system ( 3–7), and, based on animal experiments and clinical case studies ( 8–15), high-dose glucagon is recommended for reversal of cardiogenic shock induced by poisonings with cardioinhibitory drugs ( 7). Glucagon increases glucose production in the liver and is the counterregulatory hormone to insulin together, they maintain normoglycemia in the fasting state. Glucagon is secreted from the pancreatic alpha cells and possibly from enteroendocrine cells in the intestine ( 1, 2).


 0 kommentar(er)
0 kommentar(er)
